Individualized nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer
Please click here to download the model.
Background
Occult peritoneal metastasis (PM) in advanced gastric cancer (AGC) patients is highly possible to be missed on CT images. Patients with occult PMs are subject to late detection or even improper surgical treatment. We therefore aimed to develop a radiomic nomogram to preoperatively identify occult PMs in AGC patients.
Patients and methods
554 AGC patients from four centers were divided into one training, one internal validation, and two external validation cohorts. All patients’ PM status was firstly diagnosed as negative by CT, but later confirmed by laparoscopy (PM positive n=122, PM negative n=432). Radiomic signatures reflecting phenotypes of the primary tumor (RS1) and peritoneum region (RS2) were built as predictors of PM from 266 quantitative image features. Individualized nomograms of PM status incorporating RS1, RS2, or clinical factors were developed and evaluated regarding prediction ability.
Results
RS1, RS2, and Lauren type were significant predictors of occult PM (all p<0.05). A nomogram of these three factors demonstrated better diagnostic accuracy than the model with RS1, RS2, or clinical factors alone (all net reclassification improvement p<0.05). The AUC yielded was 0.958 (95% confidence interval [CI]: 0.923-0.993), 0.941 (95% CI: 0.904-0.977), 0.928 (95% CI: 0.886-0.971), and 0.920 (95% CI: 0.862-0.978) for the training, internal, and two external validation cohorts, respectively. Stratification analysis showed that this nomogram had potential generalization ability.
Conclusion
CT phenotypes of both primary tumor and nearby peritoneum are significantly associated with occult PM status. A nomogram of these CT phenotypes and Lauren type has an excellent prediction ability of occult PM, and may have significant clinical implications on early detection of occult PM for AGC.
Nomogram_OPM_AGC Version: 1.0.0
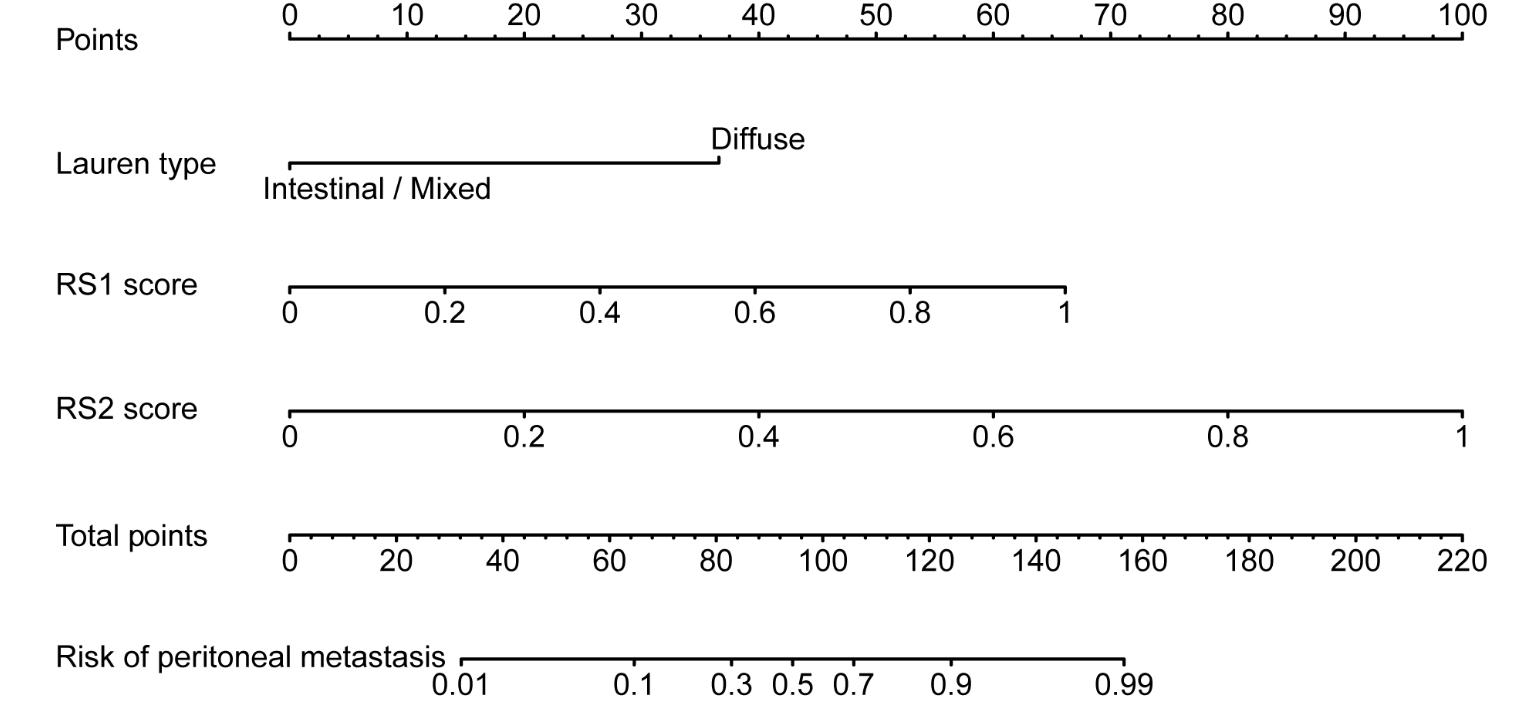
Figure 1. Radiomic nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer
Related published paper.
PURPOSE
Occult peritoneal metastasis (PM) in advanced gastric cancer (AGC) patients is highly possible to be missed on CT images, and the patients have high risk to be lately detected during the subsequent laparotomy, or worse, receive improper surgery. We aimed to develop a radiomic nomogram to identify occult PMs.
METHODS
A total of 554 AGC patients from four centers were divided into a training cohort and three validation cohorts. All patients were diagnosed as free from PM by CT, but confirmed the PM status by laparoscopy (PM positive n=122, PM negative n=432). 266 quantitative image features were extracted from both the primary tumor and nearby peritoneum region on CT. Then, radiomic signatures reflecting phenotypes of primary tumor (RS1) and peritoneum (RS2) were built as predictors of PM. An individualized nomogram incorporating RS1, RS2, and clinical factors was constructed and assessed.
RESULTS
The results revealed RS1, RS2, and the clinical factor of Lauren type were significant predictors for occult PM. The nomogram combining RS1, RS2 and Lauren type had powerful predictive ability with AUCs of 0.958 (95% confidence interval [CI]: 0.923-0.993) in the training cohort, 0.941 (95% CI: 0.904-0.977), 0.928 (95% CI: 0.886-0.971) and 0.920 (95% CI: 0.862-0.978) in the three validation cohorts. Moreover, the nomogram demonstrated better diagnostic accuracy than the model with only RS1, RS2, or clinical factors (net reclassification improvement p<0.05). Furthermore, the stratification analysis showed that our nomogram had potential generalization ability.
CONCLUSION
CT phenotypes of both primary tumor and nearby peritoneum are significantly associated with occult PM status. A nomogram based on these CT phenotypes as well as Lauren type has an excellent predictive ability of occult PM in AGC.
Citation:Di Dong#, Lei Tang#, Zi-yu Li#, Meng-jie Fang#, Jian-bo Gao#, Xiu-hong Shan#, Xiang-ji Ying, Ying-shi Sun, Jia Fu, Xiao-xiao Wang, Li-ming Li, Zhen-hui Li, Da-fu Zhang, Yan Zhang, Zhe-min Li, Fei Shan, Zhao-de Bu, Jie Tian*, Jia-fu Ji*, Development and validation of an individualized nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer, Annals of Oncology, accepted, 2018. (#these authors contribute equally to this work, *corresponding author) (SCI IF: 13.930)